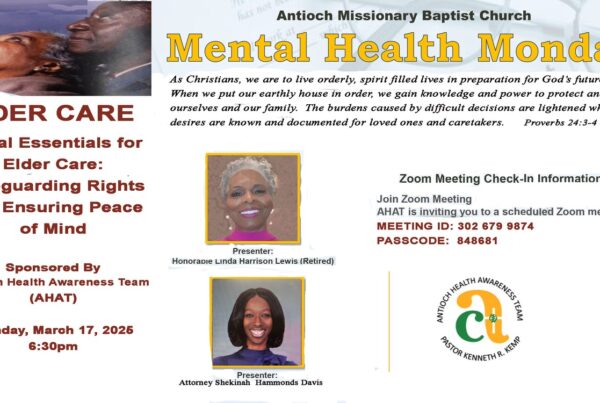
By: Shekinah Hammonds Davis
- INTRODUCTION
When the COVID 19 crisis made landfall on American soil, it seemed that patient advocacy became an unattainable goal or unreachable tool to ensure patient safety and quality continuity of care. This once shiny tool called advocacy used to bring together the professional world and laymen alike to create a bouillabaisse of solutions for patients who were not able to advocate for themselves. Once COVID 19 hit the urban and rural areas alike, the older methods that were once used to ensure patient safety, identify continuity of care, and maintain quality of care were no longer readily available because patient advocates were not allowed to physically enter health care facilities to do the work they once did. Since March of 2020, the medical profession as a whole has become strained and almost reached a breaking point to keep up with each patient’s care demands, safety in the workplace, and the pressures of prolonged staffing constraints.
Families are now feeling the sting of the lack of patient advocacy over this period where COVID 19 emerged in the medical community as a newly recognized infection. However, patient advocates can rest knowing that the laws protecting patients are still present and relevant today. This article will discuss the tools of navigating patient advocacy post COVID-19, review laws involving proper admission, transfer, and discharge planning of patients from hospitals and long-term care facilities including nursing homes, identify the pitfalls of surrogate decision making, and provide actual techniques that work and do not work with patient advocacy.
- Caveats
While patient advocacy is an extremely broad topic, this article is limited to patient advocacy in a hospital and long-term care facility setting after the COVID 19 crisis. This article will not address patient advocacy specific to minors and/or mental health patients. The rules involving certain procedures for minors and mental health patients are beyond the scope of this article and may be explored later as an addendum to this article. Special thanks are given to the Louise Batz Foundation for granting permission to use the patient advocacy manual which is found in the appendix of this paper.
This paper was written for educational purposes and should not be taken as a substitute for legal advice in any particular matter. All scenarios given were given as an example and not as a means to supplant the facts in any particular case. The suggestions made in this paper are direct suggestions the writer has used in counseling clients with effective patient advocacy and suggestions from the writer’s personal experience.
- A New Era Post-COVID 19
- Negative Effects From COVID 19
It is no secret to the healthcare community that the COVID-19 crisis has brought a great deal of uncertainty to patient care, continuity of care, and quality of care.[1] The healthcare industry has had to make changes instantaneously while responding to the strains that COVID 19 brought to patients in every care setting.[2] Patient advocates have additionally been placed in an extremely strained position by juggling federal legislation, state legislation, personal economic strains, and the ever changing rules surrounding how they communicate with healthcare professionals about a patient’ s care during the pandemic.
Some medical professions have noted that people are more emotionally reactive because of prolonged stress associated with a pandemic and the uncertainty of its end.[3] Recent studies show that older adults have reported an increase in negative mental health impacts due to the pandemic.[4] Families are not able to gather in group settings like before and the limitations on visitation into care facilities and hospitals is likely to cause “heightened risk of cardiovascular, autoimmune, neurocognitive, and mental health problems” in older adults.[5] With fewer visits from family members and loved ones, loneliness is the new pothole in patient care efficacy.
Considering current events, it is prudent as a patient advocate to locate legal documents that can facility patient advocacy in the event that you are called in to assist.
- Legal Documents to Facilitate Patient Advocacy
Just as medical professionals were required to pivot to meet the increased demands caused by the COVID 19 crisis, it is of great importance that legal professionals do the same to ensure that patients and their advocates have the proper legal protective equipment to combat the ripples of COVID 19.
To begin advocacy for a patient, a patient advocate should spend some time locating the essential tools before approaching healthcare professionals to fight for a patient’s rights. This includes locating the patient’s (1) Medical Power of Attorney,[6] (2) Durable Power of Attorney,[7] (3) Directive to Physicians and Family or Surrogates (“DNR”),[8] (4) Out of Hospital Do Not Resuscitate (“OOHDNR”),[9] (5) Declaration of Mental Health Treatment,[10] and (6) Supported Decision Making Contract.[11]
Without these documents, a patient advocate will likely experience delays in seeking treatment for the patient and could also be denied the right to review records and make decisions on the patient’s behalf. With a Medical Power of Attorney, a patient advocate can gain access to a patient’s medical records and assist with decision making as discussed below. With a DNR, a patient advocate can assist a patient in a hospital setting by asserting the patient’s original wishes regarding the continuance or discontinuance of life support when a terminal or irreversible condition is diagnosed. Without a DNR, the decision to terminate life support in a terminal or irreversible diagnosis could end up in the lap of medical staff who are not related by blood or marriage to the patient.[12]
Even a patient with a DNR should also have an OOHDNR as the latter speaks to healthcare professionals in a care facility like a DNR speaks in a hospital setting. Quite often, a resident in a care facility may experience a medical emergency that requires care facility staff to contact emergency medical services on the scene. If a paramedic responds to an emergency dispatch call regarding a resident at a care facility, they are by law required to use all methods to revive the resident. However, if a resident of a care facility has an OOHDNR that instructs the discontinuance of life support in terminal and/or irreversible conditions, a paramedic will not attempt to resuscitate the resident. This is important when a person desires to discontinue life support and does not wish to be treated in a hospital under certain conditions. This could mean that a patient may not receive cardiopulmonary resuscitation on site because emergency personnel will look to respect the patient resident’s wishes and will not use measures to resuscitate if the patient has indicated this on an OOHDNR.
Another tool that will assist a patient advocate is a Declaration of Mental Health Treatment which is codified in the Texas Civil Practice and Remedies Code.[13] This document allows a patient to designate a preferred treatment or medication in a mental health treatment setting. A patient can also use this form to list medications and treatment options that are not preferred in a mental health treatment center. This is paramount as certain medications have different effects on patients and can be more effective than others. If a patient has listed the types of medications that are not agreeable with a successful treatment plan, a patient advocate can use this document to request alternative treatment or alternative medication for the patient in a mental health setting.
A patient advocate can also use a supported decision-making contract to assist with care decisions for a patient with an intellectual disability. This form is codified in the Texas Estates Code and allows a person with an intellectual disability to name an advocate to assist them with personal, medical, and financial decisions. This document should be acknowledged by medical professionals if executed properly as is indicated by law.[14] A patient that has not executed a medical power of attorney but has executed a supported decision-making contract possesses authority to advocate for the patient in a healthcare setting depending on the authority granted by the patient.
- UNDERSTANDING THE ROLE OF PATIENT ADVOCATE
Efficacy in advocacy requires a basic understanding of each person’s role with whom the patient will encounter in the care process. The patient is likely to encounter a physician, nurse practitioner, physician’s assistant, registered nurse, licensed vocational nurse, certified nursing assistant, social worker, and other care personnel in the process of receiving care. It is important for the patient advocate to map out the team that is assigned to a patient’s care on a day-to-day basis to ensure that the notes written by the previous care professionals are properly communicated to the next staff member that enters to care for the resident/patient.
In Texas, a care facility must acknowledge the presence of a family council or the group of family and friends that take an active role in the patient’s care.[15] The purpose of the family counsel as defined by Texas law is to make recommendations to the institution proposing policy and operations decisions affecting resident care and quality of life and promote educational programs and projects that will promote the health and happiness of the resident.[16]
Many times, it is important for the patient advocate to consider bringing in the expertise of a geriatric care manager to assist with care tasks that might be overwhelming for a patient advocate. Such tasks include but are not limited to:
- Assisting with short-term or on-going assistance for long distance caregivers;
- Personalized and compassionate services focusing on individual’s wants and needs
- Manage continuity of care by facilitating family communication, reducing the burden on families and preventing unnecessary expenditures;
- Assist with efficiency and flexibility based upon client-centered approach eliminating bureaucratic constraints; and
- Helping avoid inappropriate placement.[17]
It is important to note that placement of a patient/resident is a team effort. Patient advocates set the tone of the placement because they are often the ones that can communicate the patient’s needs more completely. A geriatric care manager will look at several factors such as the income of the patient, the care needs of the patient, facility availability if Medicaid services are needed, and the overall transition process of moving a patient/resident from one location to another.
Geriatric Care Management is an unregulated term. It is always recommended to work with a Care Manager who is a member of the Aging Life Care Association (formerly the National Association of Professional Geriatric Care Managers). These professionals are held to a national Standard of Care and a Code of Ethics. They are licensed (when required in their states) and participate in annual continuing education classes. When in doubt regarding care decisions, it is always helpful to engage the assistance of a professional to ensure that the care received by the resident is the best possible solution in a care crisis.”
- Telemedicine
Among the vast changes implemented to combat COVID 19, telemedicine has emerged as the champion of healthcare for individuals that were not willing to continue the traditional visits into a doctor’s office to obtain adequate care.
Since the beginning of the pandemic, studies have documented that physicians have on average seen between 50 and 175 more patients via telemedicine than previously seen prior to the pandemic.[18] The Centers for Medicare & Medicaid Services (CMS) have made this possible by implementing changes that will compensate physicians at the same rates for services offered through telemedicine as they have done for in-person healthcare.[19] CMS also changed its policies inclusively to allow patients to see physicians via telehealth who did not have an existing relationship with the patient prior to the pandemic.[20]
The American Medical Association has gone a step further to create a Telehealth Implementation Playbook to assist physicians, care facilities, and care providers with efficacy with implementing telehealth services.[21] This implementation has increased telehealth services from an estimated $3 billion industry to a projected $250 billion industry.[22] This shift to telehealth services should help patient advocates be better advocates in that before it may not have been possible to attend an in-office doctor’s visit with the patient. Now, it is possible for patient advocates to be present virtually practically anywhere in the world with the patient if the advocate has access to the internet.
With the increased amount of telemedicine available to patients, patient advocacy is more needed now that patients can access healthcare at home. Patient advocates can utilize this shift in medicinal care to better inform physicians and healthcare professionals of the actual issues patients are experiencing. When an accurate reporter is present with a patient during a doctor’s visit, medical professionals are able to better diagnosis and furthermore treat the patient because they are being presented with accurate information about the patient’s symptoms.
Just as a patient advocate can use telehealth to assist a patient, it is equally important for advocates to know the laws that govern admissions, transfers, and discharge of a patient from a hospital or nursing care setting.
- PROPER ADMISSION, TRANSFER, AND DISCHARGE PLANNING
Patient advocacy is a valuable tool for a patient when it appears that a patient will be admitted, transferred or discharged in conflict with state and/or federal law. A hasty decision to admit, transfer, or discharge a patient without securing proper continuity of care in the new care setting is often referred to as “patient dumping” because the result of transferring a patient without a plan at the next location allows the originating facility to seemingly wash its hands clean of the patient.[23] Fortunately, there are laws against patient dumping. A patient advocate should be aware of what is required of a receiving, transferring or discharging hospital or care facility before they attempt to dump a patient at the back door of another facility. Let us first discuss the laws that govern hospitals and the impact of the “CARES ACT” on these existing laws.
- Hospital Requirements.
The CARES ACT was enacted on March 27, 2020 and included several provisions that relaxed many federal provisions to ensure that hospitals could quickly respond to the increased demand for healthcare required by the COVID 19 crisis.[24] Hospitals would need to discharge patients on a more frequent basis to protect them from COVID 19 and isolate patients who were being treated for the virus. Some advocates began to see a trend where nursing homes denied patients who were being discharged after being treated for COVID 19 in a hospital setting in fear of not wanting to potentially expose other residents to COVID 19.[25] It is important to take a moment to review what the law is on proper admissions, transfers, and discharges and how it applies to hospitals post the COVID 19 crisis.
- PATIENT’S RIGHTS.
Under Federal law, a patient has the right when admitted into a hospital to execute advance directives and have a family member or representative notified during the admission process. [26] After admission and certainly after discharge, a patient also has the right to access and obtain medical records within a reasonable time upon oral or written request. [27] This requirement however was relaxed by the enactment of the CARES ACT because during the pandemic, hospitals encountered an increased number of patients which made it difficult to be able to respond in the same manner as before to medical records requests.
In additional to the rights affording a patient under Federal Law, Texas hospitals are required to explain a patient’s rights to the patient within twenty-four (24) hours of admission into the hospital.[28] These rights must be explained to the patient in the patient’s primary language and must be signed by the patient to show receipt of said rights.[29]
- ADMISSION REQUIREMENTS.
A hospital must document and complete a medical history for each patient before twenty-four (24) hours after a patient’s admission or registration into the hospital but before surgery or a procedure requiring anesthesia service with few exceptions.[30] Additionally, the hospital must complete an updated examination of the patient, including any changes in the patient’s condition within twenty-four (24) hours after a patient’s admission or registration.[31]
Hospitals must also maintain information to justify admission and continued hospitalization, support the diagnosis, and describe the patient’s progress and response to medications and services.[32]
- OBTAINING A PATIENT’S MEDICAL RECORDS.
Although some standards have relaxed due to the enactment of the CARES ACT, hospitals must still keep records to show medical history, physical examination, admitting diagnosis, consulting evaluations, informed consent, documented complications, nursing notes, reports of treatment, medication records, lab results, vital signs and discharge summary with outcome of hospitalization, disposition of case and provisions for follow up care.[33]
As a practical tip, patient advocates should still be able to request and have access to records. However, the timeframe whereby hospitals are required to respond has lengthened to allow for proper care with current patients. A patient advocate can avoid a delay with obtaining records by keeping records in an external or electronic journal to ensure that names of the physicians, medications, and other important dates are readily accessible.[34]
- VISITATION RIGHTS.
Under Federal law, hospitals are also required to develop and post a visitation policy for families, friends and advocates visiting a patient.[35] This requirement has proven to be somewhat of a hurdle for patient advocates because since the enactment of the CARES ACT, hospitals and care facilities can restrict visitation to avoid increased patient exposure to COVID 19.[36] Without being able to go into a hospital and as one advocate stated check underneath the patient’s fingernails, a patient advocate may not be able to detect areas where patient continuity of care has fallen below the standard.
- DISCHARGE REQUIREMENTS.
When it comes to discharging a patient from the hospitals, federal law places the burden of care to develop a transition plan on hospitals to ensure that patients are not being released home without continuity of care. A patient released prematurely without a plan of care in the home could be readmitted fairly quickly if there is no plan of care prepared for at home.
To this end, a hospital must have an effective discharge plan process that focuses on patient’s goals and treatment preferences that includes the patient and the patient’s representative.[37] Hospitals are also tasked with ensuring effective transition of a patient from the hospital to a post discharge care facility or home and reduce factors leading to preventable hospital readmission.[38]
Before COVID 19, hospitals were also required to include post-hospital services in all discharge plans to include hospice services, home health care, community providers, and ensure that the patient had access to these services prior to being discharged.[39] The CARES ACT suspended this requirement for hospitals that provide critical care for patients due to the volume of patients that were being cared for during the COVID 19 health crisis.[40] Paramount to patient care is the requirement that hospitals must discuss these choices with the patient and the patient’s representative to ensure that the patient is informed of follow-up care.[41]
In Texas, a discharge plan from a hospital in Texas must additionally include a written continuing care plan that address the patient’s needs for care after discharge which includes the contact information for the doctor, contact information for the patient’s representative, any advance directives executed by the patient, special instructions or precautions for ongoing care, comprehensive care plan goals, and a discharge summary.[42] Additionally, the discharge plan must include recommendations for treatment and care and information about the availability of resources for treatment of care. Discharge documents must also include the following:
- Basis for the transfer;
- List the specific needs that cannot be met by the current hospital;
- Attempts made by hospital to meet patient’s needs; and
- Services available at the new hospital or facility to meet the needs of the patient.[43]
Discharging a patient additionally requires that a written continuing care plan be provided to the patient, the person designated by the patient, and upon request to a family member, guardian, or individual who has demonstrated on routine basis responsibility and participation in the patient’s care and treatment.[44] It is important to note that this can be provided to the patient up to two (2) days after the discharge date if requested.[45]
As a practical matter, if you are assisting a family advocate or patient with obtaining details about an admission, transfer, or discharge decision made by the hospital and the nursing staff do not wish to reconsider the admission, transfer, or discharge decision, consider appealing the decision to the hospital’s board of ethics to ensure that the patient receives a fair review of the medical decision made that involves admission, transfer, or discharge.
- Nursing/Care Facility Requirements.
The issue of patient dumping is also seen in the nursing care facility arena because nursing home administrators are required to follow the law when it comes to admitting, transferring or discharge a resident from their facility. Some advocates report that there were a hand full of nursing homes that wrongfully denied a patient’s admission in fear of inadvertently brining a COVID 19 patient into the care facility.[46] Other advocates discovered that there was a group of nursing home administrators that sought to admit extremely ill patients for a short period of time during the COVID 19 crisis because they could get more money for treating several extremely ill patients for a short time than if they had admitted one stable patient.[47] It is important that patient advocates understand the rights afforded to patients under Federal and Texas law in these situations to ensure proper patient continuity of care.
By law, a nursing care facility must ensure equal access to quality care by establishing, maintain and implementing identical policies and practices regarding transfer and discharge regardless of source of payment.[48] Similar to hospitals, a nursing care facility must have an admission policy and must not require residents to waive their rights under Federal or State law to be admitted.[49] Also on the “thou shalt not” list is a facility may not require oral or written assurance that a resident or potential resident is not eligible or will not apply for Medicare or Medicaid benefits.[50]
Common in the admission process is a desire by the facility to name someone who will be financially responsible for the bill should the primary or secondary payor fail to remit payment. Federal law prohibits a facility from requesting or requiring that a third-party become the guarantor of any debt incurred by the patient and makes the guarantee a condition of admission or expedited admission or for a resident’s continued stay.[51]
A facility may however ask the legal representative of the patient to sign and guarantee payment from the resident’s personal funds.[52] As a practical note, it is important that a patient advocate that executes documents on behalf of a patient ensures that their signature bears the endorsement of the representative on behalf of the resident in their “representative capacity” by writing their title next to their signature. This ensures that the facility is put on notice of the representatives’ role on behalf of the resident.
A patient advocate should also be alert and vigilant to read the admission paperwork because a care facility may not request or require residents or potential residents to waiver potential facility liability for losses of personal property.[53] Finally, a facility must not charge, solicit, accept, or receive, in addition to any amount otherwise required to be paid under the state plan any money as a precondition of admission or continued stay for persons eligible for Medicaid.[54] It is imperative to note that a facility may charge a resident that receives Medicaid for incidentals provided by the facility.[55]
- CARE PLAN.
Federal law provides that a facility must develop a baseline plan of care for each resident that includes the instructions needed to provide effective person-centered care of the resident.[56] This plan must be developed within forty-eight (48) hours of admission, include minimum healthcare information necessary to properly care for a resident including but not limited to the following:
- Initials goas based on admission orders;
- Physician orders;
- Dietary orders;
- Therapy services; and
- Social Services.[57]
In Texas, the Plan must include documents regarding the patient’s status in relationship to goal attainment.[58] The care plan team should conference at least once every quarter to determine the appropriateness of treatment.[59] The Plan must also articulate the initial goals of the resident, a summary of the resident’s medications and dietary instructions, any services and treatments to be administered by the facility and any updated information based on the details comprehensive plan.[60]
- TRANSFER AND DISCHARGE.
A nursing care facility must only transfer or discharge a patient when there are specific reasons to discharge which are permitted under federal law. A facility may not transfer or discharge a patient from a nursing care facility unless
- Transfer or discharge is necessary for the resident’s welfare and the needs of the resident cannot be met at the current facility;
- Transfer or discharge is appropriate because the resident’s health has improved sufficiently so the resident no longer needs the services provided by the facility;
- The safety of individuals in the facility is endangered due to the clinical or behavioral status of the resident;
- The health of the individuals in the facility would otherwise be endangered;
- The resident has failed, after reasonable and appropriate notice to pay for (or to have paid under Medicare or Medicaid) stay at the facility; or
- When the facility ceases to operate.[61]
If a resident appeals the decision of the facility to discharge the resident, the facility may not transfer or discharge the resident during that process unless failure would endanger the health and safety of the resident or other individuals in the facility.[62] The facility must document the danger that failure to transfer or discharge would pose.[63] As a practical matter, it is important for the advocate to seek new placement for a resident if the facility requests transfer to ensure that the resident receives the best quality of care during the transition period.
Similar to hospital discharge orders, a discharge order from a nursing care facility must describe the basis for the transfer, list the specific needs that cannot be met by the facility, attempts made by the facility to meet the resident’s needs, and services available at the new facility to meet those needs.[64]
Finally, discharge orders must include contact information from the physician signing the discharge, the contact information for the resident’s representative, any advance directives received on behalf of the patient, special instructions or precautions for ongoing care, comprehensive care plan goals, and a discharge summary.[65] This notice must be given to the resident with at least thirty (30) days advance notice of discharge.[66] Patient advocates should be aware of these statutes to enforce the notice requirements should a facility insist on discharging a patient contrary to federal or state law.
- SURROGATE DECISION MAKING
When treating a patient, medical professionals are to primarily seek permission and informed consent from the patient to whom will receive the medical services. However, there are times when a patient lacks capacity to make that decision and a surrogate decision maker must asset their right to assist with care or treatment decisions. The law is slightly different when it comes to who has priority to make decisions regarding (i) medical treatment, (ii) surgery and invasive procedures, and (iii) end of life decisions. Patient advocates should be aware of who has priority to serve as a “surrogate” so that they can step in to assist with decision making at the right time for a patient.
- Medical Treatment.
As is expected, if a patient is in need of basic medical treatment or the administration of general medication which is not considered invasive or surgical in nature, a patient with capacity to make an informed decision has the right to consent to receive or deny medical services.[67] If a patient lacks capacity to make this decision, then medical personnel will look to a person who possesses a Medical Power of Attorney to make this decision.[68] If there is no designated Agent under a Medical Power of Attorney, then the following persons have priority to assist the patient in this order with the first person having the highest priority with decisions for the patient regarding medical treatment:
- The Patient’s spouse;
- An adult child of the patient who has the waiver and consent of all other qualified adult children of the patient to act as the sole-decision maker;
- The majority of the patient’s reasonably available adult children;
- The patient’s parents;
- The individual clearly identified to act for the patient by the patient before the patient’s became incapacitated, the patient’s nearest living relative, or member of the clergy.[69]
Please note that a surrogate decision maker cannot consent to voluntary inpatient mental health services, electro-convulsive treatment, or appoint another to make surrogate decisions.[70] As a practical matter, the patient should name an alternate agent should the primary agent be unavailable to act on behalf of the patient. If anyone disagrees with the decisions made by the physician or the surrogate decision maker, a temporary guardianship must be obtained to resolve the conflict.[71]
- Surgical and Invasive Consent
If a patient requires any type of invasive or surgical procedures, the decision to proceed still rests with the patient followed by the Agent under a Medical Power of Attorney.[72] If the patient is unable to make this decision and lacks an Agent, then the list of priority changes slightly when making these decisions. For procedures that are considered major medical or dental treatment, a surrogate in the order of priority may assist with making these decisions:
- Actively involved spouse;
- An actively involved adult child who has waiver of all other actively involved adult children of the client to act as sole decision-maker;
- An actively involved adult sibling who has the waiver and consent of all other actively involved adult siblings; or
- Any other actively involved adult relative who has the waiver and consent of all other actively involved adult relatives of the patient.[73]
It is important to note that this statute adds the term “actively involved” to each of the named persons who may serve as a surrogate. This seems to suggest that an estranged spouse, child, adult sibling, or relative should not be making surgical decisions on behalf of a patient. A patient advocate that may have lower priority in the statute but is actively involved may be able to use this portion of the statute to support their right to make surgical decisions in the event that a person who is not active but with higher priority desires to make these decisions.
- End of Life Decisions
As was established with decisions involving medical treatment and invasive and surgical procedures, the patient has the primary right to make the decision to continue or terminate life support when diagnosed with an irreversible or terminal condition. These decisions are hereinafter referred to as “end of life decisions.” If the patient is unavailable to make this decision, medical personnel will then attempt to ascertain the patient’s desires as is stated on a DNR.[74]
If a patient has not signed a DNR, the patient’s treating physician and a Guardian may make this decision for the patient.[75] If the patient has no Guardian, then the treating physician and the agent under a medical power of attorney signed by the patient may make this decision on behalf of the incapacitated or unresponsive patient.[76] If the patient failed to name an agent under a medical power of attorney, then the treating physician along with one person listed below may make the decision on behalf of the patient in this order of priority:
- Patient’s spouse;
- Patient’s reasonably available adult children;
- Patient’s Parents;
- The patient’s nearest living relative; or if no one able is available, then
- An attending physician who is not involved with the day to day treatment of the patient or a member of the ethics committee of the facility.[77]
Patient advocates who are not in this list who are not family members will not be able to exclusively make this decision. If a patient seeks to have a friend advocate make this decision, please advise your clients that they must do so in advance by delegating that authority in a medical power of attorney or executing a DNR on behalf of the patient.
- Do’s and Don’ts of Patient Advocacy
As a patient advocate, it is important to understand the current state of healthcare affairs, key players who facilitate patient safety, and the laws surrounding patient’s rights. With this information comes great responsibility to do all you can do by using the tools of patient advocacy to seek the best treatment for a patient. However, there are a list of things that an advocates can do unintentionally which can cause angst in the care plan and ultimately will not lead to effective advocacy for the patient. Before discussing the Do’s, it is worth discussing the techniques that do not work when advocating for a patient.
- The Don’ts.
There are things that patient advocates do unintentionally that ultimately cause strife in a care team and at the top of the list is poor communication. Effective communication is an art because it requires gentle or deliberate strokes of using words, expressions, and actions to communicate a concept to the receiving party. Just as you would when painting an original portrait or painting on canvas, the colors you use, the type of brush used, and the mixture of the two can create a masterpiece that is unforgettable.
It is imperative that patient advocates start with good communication when advocating on behalf of a client. Communication that involves increasing the volume of your voice, anger, or legal threats do not give the patient the best chance of getting expedited care.
It is often frustrating when communicating with a member of a care team that refuses to consider the patient’s needs as primary in the care spectrum. However, as a patient advocate, it is helpful to you and the patient to not misquote the law and quite frankly loose your temper on care professionals because temperament is everything when advocating for a patient. Remember that your attitude can impede care on behalf of the patient if you allow your temperament to cloud your judgment.
- The Do’s.
While there are things that are likely to cause strife in a care team, there are things that a patient advocate can do that can pull together a care team on behalf of a patient. Some have said “patience is a virtue.” However patience in patient advocacy does not comport to waiting on the sidelines until you hear an answer from the care team. Patience in patient advocacy is simply taking the time to understand the different perspectives while understanding that the medical community is under extreme stress.
By exhibiting patience, a patient advocate can take good notes and be willing to allow the care professionals a reasonable time to return with accurate information. In a post-COVID 19 world, delays are expected in hospital and care facility. However, a patient advocate should be patient to allow the care team time to consider all options that would be beneficial to the patient.
Another tool that is helpful in patient advocacy is keeping good notes. A patient advocate should have the ability through an advocacy tool such as the Batz Guide included in the APPENDIX to keep up with the patient’s medical notes because it is likely that the patient that is being treated will not remember everyone that visits, nor will they remember the results of every test. A patient advocate that keeps copious notes is more likely to identify a problem or a break in care when it occurs.
Lastly, patient advocates should master the art of saying, “thank you.” Many times the patient advocate acts as the voice for the patient. Appreciating medical professionals, staff members, and even the janitor can open the doors of communication for the patient and people are more likely to work efficiently when they feel they are being appreciated. If you make it a habit to show gratitude to the staff that provide care, it speaks volumes on behalf of the patient as the patient may not be able to show gratitude due to their condition. If you take time to complain, it is important to also take time to express gratefulness as well.
- Conclusion
Patient advocacy requires collaboration of the care team which includes the advocate to develop the best possible treatment or recovery plan that is possible for the patient. Patient advocates should work to locate the necessary documents needed that will assist them with obtaining information, records, and making medical decisions. If a patient advocate is denied the rights to assist on behalf of a patient, they should understand the order of priority of persons who have the right to make these decisions on behalf of a patient. Lastly, patient advocates should use the tools that are effective in patient advocacy and avoid the pitfalls of advocating on behalf of a patient. Patient advocates are guardian angels for a patient as they guide care, they direct treatment and ultimately speak on behalf of patients that have no audible voice to communicate their wishes with the care team.
APPENDIX
- Louise Batz Guide for Patient Advocacy
- Medical Power of Attorney
- Durable Power of Attorney
- Directive to Physician and Family or Surrogate
- Out of Hospital Do Not Resuscitate
- Declaration of Mental Health Treatment
- Supported Decision Making Contract
[1] Muchmore, Shannon, “Hospitals Dipping Into Emergency Stocks to Combat Coronavirus,” March 10, 2020, https://www.healthcaredive.com/news/hospitals-dipping-into-emergency-stocks-to-combat-coronavirus/573804/; Feuer, Will, “CDC Says New Covid Strain Could Further Stress ‘already heavily Burdened’ Hospitals,” December 30, 2020, https://www.cnbc.com/2020/12/30/cdc-says-new-covid-strain-in-us-could-stress-heavily-burdened-hospitals.html.
[2] Id.
[3] Javed, Bilal, et al, “The Corona (COVID 19) Pandemic’s Impact On Mental Health,” June 22, 2020, ©2020 John Wiley & Sons, Ltd, https://onlinelibrary.wiley.com/doi/full/10.1002/hpm.3008.
[4] Panchal, Nirmita, et al, “The Implications of COVID-19 for Mental Health and Substance Use, August 21, 2020, https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/.
[5] Armitage, Richard, et al, “COVID-19 and the Consequences of Isolating the Elderly,” May 5, 2020, https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/.
[6] See Texas Health and Safety Code § 166.164 for statutory form.
[7] See Texas Estates Code § 751.051 for statutory form.
[8] See Texas Health and Safety Code § 166.033 for statutory form.
[9] See Texas Health and Safety Code § 166.082 for statutory form.
[10] See Texas Civil Practice and Remedies Code § 137.011 for statutory form.
[11] The Texas Health and Human Services offers a template to assist Texas residents with preparation of a Medical Power of Attorney, Durable Power of Attorney, Out of Hospital Do Not Resuscitate, and Declaration of Mental Health Treatment. See https://hhs.texas.gov/laws-regulations/forms/advance-directives. The Supported Decision Maker Contract can be found in Section 1357.056 of the Texas Estates Code. A sample form for each of these documents can be found in the Appendix of this article.
[12] See Texas Health and Safety Code § 166.039(e).
[13]Id at 10.
[14] See Texas Estates Code § 1357.001 et. seq.
[15] Tex Health & Safety Code § 242.901-906.
[16] Tex. Health & Safety Code § 242.902.
[17] https://www.aginglifecare.org/.
[18] Zarefsky, Marc, “5 Huge Ways the Pandemic Has Changed Telemedicine,” August 26, 2020. See https://www.ama-assn.org/practice-management/digital/5-huge-ways-pandemic-has-changed-telemedicine.
[19] See MEDICARE TELEMEDICINE HEALTH CARE PROVIDER FACT SHEET | CMS, www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet .
[20] See Section 4401 et. seq. of the Coronavirus Aid, Relief, and Economic Security Act (“CARES Act”), https://www.congress.gov/bill/116th-congress/senate-bill/3548/text?q=product+actualizaci%C3%B3n.
[21] AMA® Telehealth Implementation Playbook | AMA (ama-assn.org), https://www.ama-assn.org/system/files/2020-04/ama-telehealth-playbook.pdf.
[22] Bestsennyy, Oleg, Gilbert, Greg, Alex Harris, and Rost, Jennifer, “Telehealth: A Quarter-Trillion Dollar Post-COVID-19 Reality?” See https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality.
[23] Galvin, Gaby, “’Patient Dumping’ Still A Problem Despite Law, “ US NEWS, April 1, 2019, https://www.usnews.com/news/health-news/articles/2019-04-01/patient-dumping-still-a-problem-despite-federal-law.
[24] See https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf.
[25] Graham, Judith, “Coronavirus Patients Caught in Conflict Between Hospital and Nursing Homes,” March 30, 2020, KHN, https://khn.org/news/coronavirus-patients-caught-in-conflict-between-hospital-and-nursing-homes/.
[26] 42 CFR 482.13(b)(3).
[27] 42 CFR 482.13(d)(2).
[28] Texas Administrative Code § 133.42(b)(3).
[29] Id.
[30] 42 CFR 482.22(c)(5)(i).
[31] 42 CFR 482.22(c)(5)(ii).
[32] 42 CFR 482.24(c).
[33] 42 CFR 482.24(c)(4).
[34] See Appendix for a copy of the Louise Batz Guide for Patient Advocacy which is an excellent organizational guide in workbook form which helps patient advocates keep track of records during a hospitalization. This resource can also be found in in an electronic application or hardcopy form. For more information, please visit https://www.louisebatz.org/.
[35] 42 CFR 482.13(h).
[36] See https://www.cms.gov/files/document/covid19-emergency-declaration-health-care-providers-fact-sheet.pdf related to patient visitation.
[37] 42 CFR 482.43.
[38] Id.
[39] 42 CFR 482.43(a)(1).
[40] 42 CFR 485.642; See also https://www.cms.gov/files/document/covid19-emergency-declaration-health-care-providers-fact-sheet.pdf.
[41] 42 CFR 485.642(b).
[42] Texas Administrative Code § 133.41 (c)(8).
[43] 42 CFR 482.43.
[44] Texas Administrative Code § 133.41 (c)(8)(C).
[45] Id.
[46] Graham, Judith, “Coronavirus Patients Caught In Conflict Between Hospital and Nursing Homes, March 30, 2020, https://khn.org/news/coronavirus-patients-caught-in-conflict-between-hospital-and-nursing-homes/.
[47] Silver-Greenberg, Jessica, “They Just Dumped Him Like Trash’: Nursing Homes Evict Vulnerable Residents,” New York Times, June 21, 2020, https://www.nytimes.com/2020/06/21/business/nursing-homes-evictions-discharges-coronavirus.html.
[48] 42 CFR 483.15 (b).
[49] 42 CFR 483.15 (a)(2)(i).
[50] 42 CFR 483.15 (a)(2)(ii).
[51] 42 CFR 483.15 (a)(3).
[52] Id.
[53] 42 CFR 483.15 (a)(2)(iii).
[54] 42 CFR 483.15 (a)(4).
[55] 42 CFR 483.15 (b)(2).
[56] 42 CFR 483.21.
[57] Id.
[58] Texas Administrative Code § 19.801(1)(A).
[59] Texas Administrative Code § 19.801(3).
[60] Texas Administrative Code § 19.802(a)(3).
[61] 42 CFR 483.15(c)(1)(a)-(f).
[62] Id.
[63] 42 CFR 483.15(c)(2).
[64] 42 CFR 483.15(c)(2)(i)(B); and TAC 19.803.
[65] 42 CFR 483.15(c)(2)(iii).
[66] 42 CFR 483.15(c)(4)(i).
[67] Texas Health & Safety Code 313.004(a).
[68] See the Texas Medical Power of Attorney form found in Texas Health & Safety Code 166.164.
[69] Texas Health & Safety Code 313.004(a)(1)-(5).
[70] Texas Health & Safety Code 313.004(d).
[71] Texas Health & Safety Code 313.004(b).
[72] Id at 70.
[73] Texas Health & Safety Code 597.041.
[74] Texas Health and Safety Code 166.039(a).
[75] Id.
[76] Id.
[77] Texas Health and Safety Code 166.039(b).